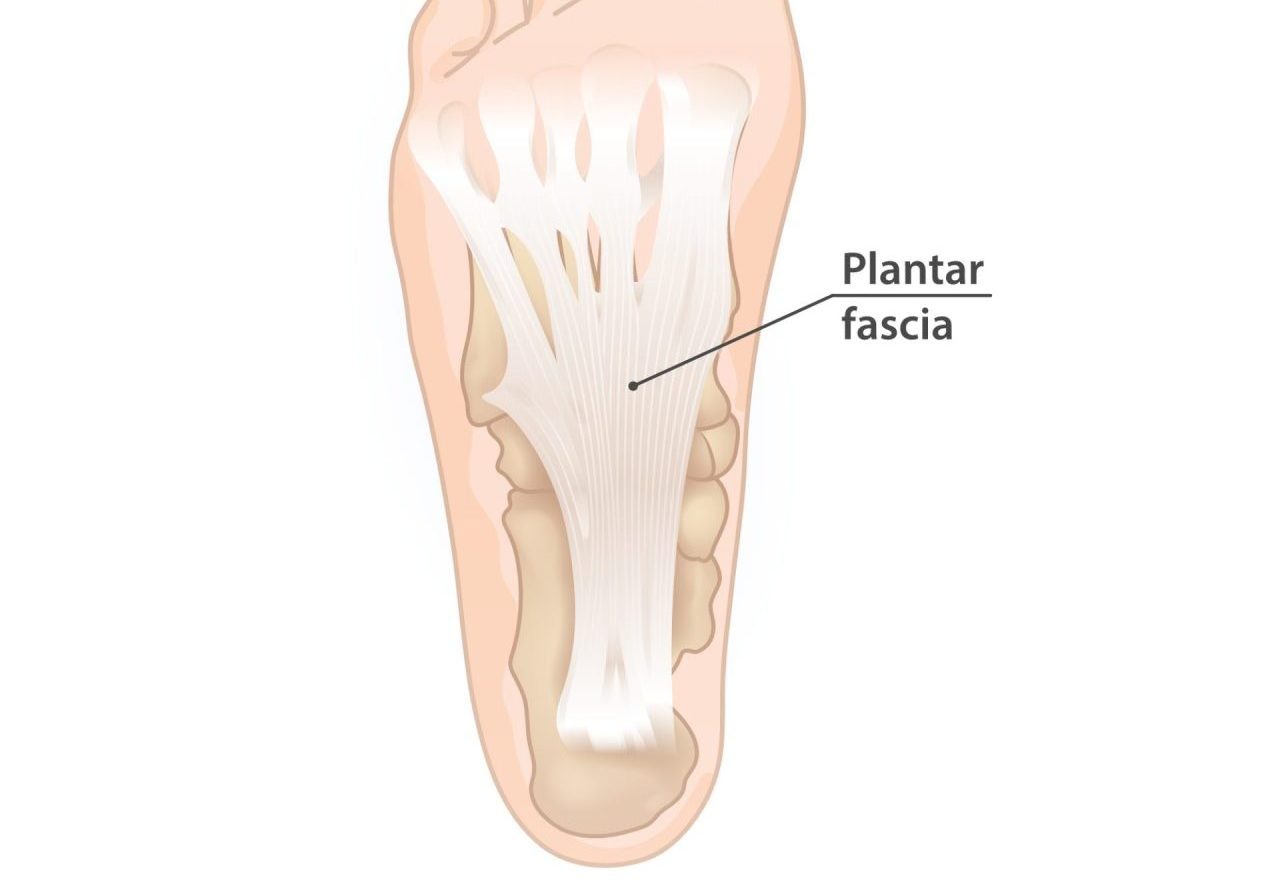
Plantar fasciitis is a condition that causes heel pain, specifically at the bottom of the foot near the heel. It occurs when the plantar fascia, a thick band of tissue that supports the arch of the foot, becomes inflamed and irritated. This condition occurs when the plantar fascia is overloaded, this can be due to an increase in load through the foot, repetitive strain, excessive foot pronation, poor footwear, or tight calf muscles.
Managing plantar fasciitis requires a comprehensive approach to reduce pain, promote healing, and restore function. By applying the 5 stages of rehabilitation, individuals with acute plantar fasciitis can effectively recover and regain optimal foot health. Chronic or persistent plantar fasciitis often responds well to shockwave therapy.
- Pain management: The first stage focuses on managing pain and reducing inflammation in the affected foot. Physiotherapists may employ treatments such as muscle release, supportive taping, ice therapy, heat therapy, or shockwave therapy to alleviate pain and promote healing. They may also recommend over-the-counter medications, if necessary, to manage pain, inflammation and discomfort.
- Range of motion: Once pain is under control, the emphasis shifts to restoring normal range of motion in the foot and ankle. Physiotherapists prescribe gentle stretching exercises to improve flexibility and reduce tension in the plantar fascia. These exercises may aim to increase the flexibility around the foot and ankle (calf muscles, foot and toe muscles) or the plantar fascia itself depending on where stiffness is identified.
- Motor control and foot mechanics: This stage focuses on improving motor control and optimizing foot mechanics to reduce strain on the plantar fascia. Physiotherapists assess gait patterns and foot mechanics and may recommend orthotics or shoe modifications to provide better support and alignment. They also prescribe specific exercises to strengthen the intrinsic foot muscles and improve overall foot stability.
- Strengthening and stability: Strengthening the muscles of the foot and lower leg is crucial for providing support and stability to the plantar fascia. Range Physiotherapists will design a personalized exercise program that targets the intrinsic foot muscles, calf muscles, and other lower leg muscles. These exercises may include toe curls, calf raises, foot arch strengthening exercises, and other specific strengthening exercises to gradually build strength and stability.
- Maintenance and prevention: The final stage focuses on maintaining the gains achieved through rehabilitation and implementing strategies to prevent future episodes of plantar fasciitis. Range Physiotherapists will provide guidance on proper footwear, orthotics, and modifications to prevent excessive strain on the plantar fascia. They may also advise individuals on stretching and strengthening exercises to incorporate into their regular routine to maintain foot health and prevent recurrence.
Working closely with a qualified physiotherapist who specializes in foot and ankle rehabilitation is crucial. Range Physiotherapists will assess the severity of the plantar fasciitis, develop a personalized treatment plan based on the 5 stages of rehabilitation, and monitor progress throughout the process. At times plantar fasciitis progress can seem slow, Range Physiotherapists can advise when seeking additional interventions, such as shockwave therapy, injection therapy or even surgery would be appropriate. With proper treatment, exercises, and adherence to preventive strategies, individuals with plantar fasciitis can experience pain reduction, improved foot function, and a reduced risk of recurrence.
For more information regarding plantar fasciitis please see: https://www.healthdirect.gov.au/plantar-fasciitis