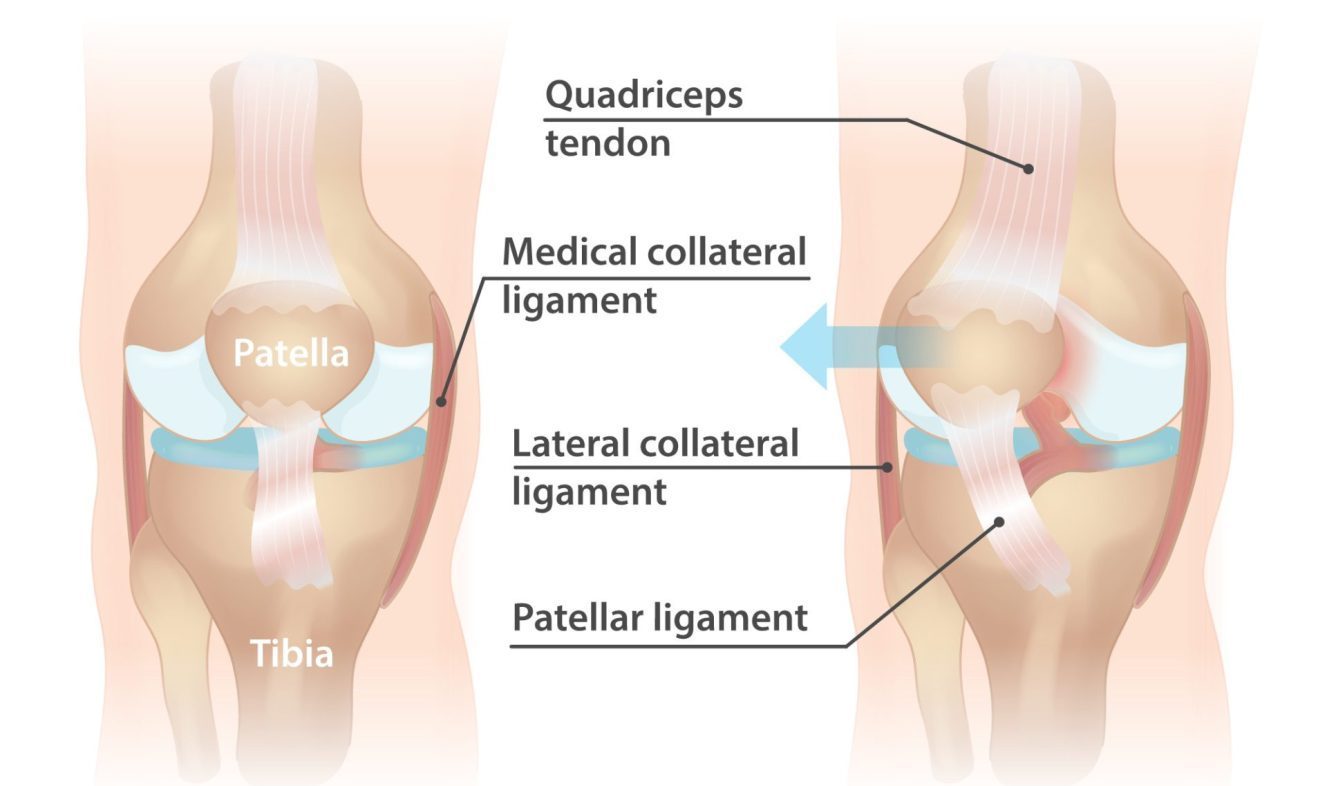
Patella dislocation occurs when the kneecap (patella) slips out of its normal position, usually towards the outer side of the knee joint. This can occur as a result of sudden twisting or direct impact to the knee, or from an underlying anatomical abnormality. Patella dislocation is more common in young athletes and females.
Symptoms of patella dislocation may include pain, swelling, and instability in the knee joint. In more severe cases, the patella may visibly dislocate and need to be manually manipulated back into its proper position. In some cases, there may also be damage to the surrounding ligaments or cartilage.
Treatment for patella dislocation typically involves a combination of physiotherapy, medications, bracing, and in some cases, surgical intervention. The decision to undergo surgery will depend on the severity and frequency of dislocations, the patient’s age and activity level, and the extent of any additional knee damage. Physiotherapy is an important component of pre- and post-operative care and can help to promote healing, reduce pain and inflammation, and restore function and mobility in the knee joint.
Applying the 5 stages of rehab to patella dislocation can help achieve the best possible outcome as follows:
Pain and symptom management: The primary goal is to reduce pain and inflammation. Rest, ice, compression, and elevation (RICE) are often recommended in the initial stages of treatment. Pain-relieving medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to manage pain and reduce inflammation. Physiotherapy treatments such as ultrasound, soft tissue massage, and taping can also help to reduce pain and swelling.
Range of motion. Once pain and inflammation are under control, the focus shifts to restoring normal range of motion in the knee joint. Physiotherapy treatments such as gentle mobilization, stretching exercises, and joint mobilization techniques can help to improve flexibility and reduce stiffness in the knee joint.
Motor control. In stage 3, the focus is on improving neuromuscular control around the hip, knee, and ankle joints. Exercises that target the muscles around the knee joint, including the quadriceps, hamstrings, and calf muscles, can help to improve knee function immediately following injury. It is important that the muscles around the hip and ankle are also addressed at this stage, as they influence how load / force is applied to the knee, particularly twisting forces.
Strengthening. In stage 4, the goal is to build strength in the muscles around the knee joint to improve stability and reduce the risk of reinjury. Resistance training, including exercises such as squats, lunges, and leg presses, can help to build muscle strength and endurance. Plyometric exercises, which involve jumping and landing, can also help to improve power and explosiveness in the lower limb muscles.
Maintenance. In the final stage of rehab, the focus is on maintaining the gains achieved in the previous stages and preventing reinjury. This may involve continuing with regular exercise, including strengthening and proprioceptive training, as well as making necessary modifications to daily activities or sports participation to reduce the risk of further injury.
In addition to rehab exercises, a knee brace may be recommended to support the knee joint and prevent future dislocations. In some cases, surgery may be necessary to repair any damage to the knee joint, such as a torn ligament or cartilage. Your physiotherapist will work closely with your doctor or surgeon to develop an individualized treatment plan to help you recover from a patella dislocation and return to your desired level of activity.